A lot has happened since my last post. I have had my fourth breast cancer operation, my lovely friend John (that I’ve known since childhood), died and I’ve had four cycles of chemotherapy. I think it is fair to say I have been holding on….
Holding on to the lifestyle I had carved for myself.
Each surgical operation I have had through this breast cancer journey has had this habit of bringing with it another additional bit of bad news. A kind of tortuous drip effect, we (my husband and I) have adjusted to the tumour status and characteristics at each investigation or operation outcome. Going into the last operation I had hoped we knew everything we needed to know. However, pathology reports have this habit it seems (in my case anyway) of churning out more findings; this time it was additional tumour and another positive axillary lymph node. We reset our mark in the sand again and after a short period of psychological adjustment, we recalibrate, recover and carry on.
Body changing and life changing surgery takes a while to adjust to. Having all of your lymph nodes removed from your axilla means you are forever at risk of arm lymphoedema. This means that you can no longer have any blood tests, injections or blood pressure measurements taken on that arm. Not much of an issue you might think, but it means the other arm as a consequence takes the full assault of tests and has consequences for subsequent chemotherapy administration. It also means you have arm exercises that you must do for life. Recovery from surgery can seem to take forever, regaining full arm movement is a slow process that takes perseverance. In reality, it wasn’t that bad for me and I managed to get back into handstand (it was a personal goal) about 4 weeks post-surgery; recovery isn’t all bad news.
Coming to terms with an altered body image has been a longer journey. My surgeon did an amazing job for me and I am very happy with the overall cosmetic result. Wearing a bikini on holiday this summer wasn’t an issue for me. Strangely, it has been managing the process of showering and getting changed at the gym that has been a challenge. Gym life BC (before cancer) I would undress with gay abandon in the changing room, my philosophy, we all have bodies they’re just different shapes and sizes-no big deal. Gym life post cancer surgery, yeah not so much gay abandoning going on here. In an effort to retain some aspects of the lifestyle I had BC I was desperate to get back to the gym, but the anxiety of changing in the wide-open space of the gym changing room was becoming an easy excuse to avoid the gym altogether. It can seem such a small thing in the big scheme of things, but being able to overcome those anxieties and feel able to do normal very basic activities I’d previously not blinked an eye about, is a big deal when sport and exercise is a big part of who you are.
Moving on to chemotherapy, I knew having chemotherapy would be tough, I’ve talked to plenty of cancer patients over the years. I’m also very resilient and a pretty tough cookie. I managed to get to the level of third Dan black belt in karate (not quite sure how, except for the expert instruction from the superb Sensei Matt Price and Sensei Nick Heald from the Leeds Karate Academy). I’ve taken plenty of punches (and kicks) over the years and I know I can take pain and not even wince. Yet chemotherapy is really tough, the physical side effects are managed really well by the team of professionals looking after me, but managing chemotherapy and life, and work has been extraordinarily rough. At the first chemotherapy cycle it took the expert nurses four attempts to put a cannula in my left arm to administer the drugs; I knew it was going to be an issue as even the experienced anaesthetist at my last operation had struggled to get a cannula in first time. So, we’d gone to my first chemo session prepared. My husband had me warming up at home to get my blood vessels working and this continued once we arrived on the chemo unit. Picture this, me in my little Ted Baker off the shoulder dress and heels (it was August and still warm) my husband has me doing squats and lunges in my chemo bay in the off the shoulder dress and heels while we wait the arrival of the chemotherapy drugs from pharmacy. Yes, I drew a few looks, but I was eventually cannulated and we were off. This is me at cycle one wearing the very attractive cold cap in an attempt to reduce the impact of hair loss.

I had thought I knew quite a lot about chemotherapy given my professional background, yeah, strike that, I now know I knew very little. When you have chemotherapy, your immune system is compromised and so you are vulnerable to picking up infections you would normally fight quite easily. To reduce the risk of developing a bacterial infection you are advised to avoid certain foods, the list is way longer than I expected. I also didn’t realise that the chemotherapy would have such an impact on the veins in my left arm as quickly as it did. By cycle 2 I was already feeling pain in my lower arm on administration of the drugs and afterwards this discomfort continued. With the support and expertise of the Oncology nurses I moved to having a PICC line inserted (Peripherally Inserted Central Catheter) and this has made subsequent chemotherapy administration much easier. PICC lines are not without their problems though, they have to be managed carefully to avoid them becoming blocked and infected (weekly flushing and dressing changing) and they must be kept dry. I was given a plastic sleeve to support showering with the PICC line and advised that many patients find wrapping the arm in cling film often works better. Try wrapping yourself in cling film with one hand it’s not easy and it didn’t go well for me. Needless to say, I’ve stuck with the plastic sleeve..
The main learning for me has been about the cold cap used to support patients having chemotherapy to keep their hair. For instance, I didn’t know that around half of people that try the cold cap are unable to tolerate it (people who suffer from headaches can find it unbearable). The cold cap success rates also aren’t as great as some of the reports on the internet suggest. Even if you can tolerate it, it doesn’t work for everyone and it depends on the type of chemotherapy drugs you are prescribed and even for women having chemotherapy for breast cancer the drugs you are prescribed can vary. You also have to wear the cold cap prior to administration of the chemotherapy (approximately 30minutes before) and for a period of time after chemotherapy has been given (around 90 minutes afterwards), it basically can feel like a long time.
Trying to hold on to my hair.
I had tried the cold cap for the first 2 cycles but it didn’t work for me, and losing my hair was traumatic despite being prepared that the cold cap might not work. I suffered depression after cycle 2. I didn’t want to get out of bed, I didn’t want to see anyone or talk to anyone and I was ready to give up. My friends were messaging me as they were worried as I’d stopped doing drop offs and pick-ups at gymnastics, I avoided everybody including my sister who has been a pillar of support through my whole cancer journey. I was lucky to have the amazing support from my hairdresser and friend of over ten years who skilfully managed my collapse from “I can do this bring it on” to “I can’t face this, it’s too much”. My hair had dropped out in clumps it was uneven with bald patches in weird places and we both finally agreed the best course of action was to shave the remaining hair off. So, one Sunday afternoon that’s exactly what she did for me. Getting myself there and managing to sit there while she shaved what was left of my hair was so difficult, and I only managed it because of her love and care. The task of ringing up and booking an appointment to get a wig was another unbelievably hard step for me to take.
You might wonder why losing your hair could be such a big deal given the other things cancer puts you through. Everyone is different, and for me it was a big deal. I’ve never been a very confident person. As a small child I was extremely shy and I found it hard to talk to anyone I didn’t know well. On my first day of clinical placement as a student therapeutic radiographer at The London Hospital, I was so nervous about speaking to patients I lost my voice (I’d not been ill) I was simply overwhelmed by anxiety; I overcame this fear as my student training progressed. As I moved into the role of a qualified health practitioner I developed strategies to enhance my confidence; I worked hard to make sure my professional knowledge was sound so I could talk with confidence at work, and I wore my hair in different ways to express the inner me and to boost my self-worth. These strategies have continued as I transferred into a lecturer and researcher role. Standing in front of large audiences to speak can be daunting and feeling prepared has gone hand in hand with feeling well presented and having good looking hair. More than that even, I love visiting my hairdresser, she’s a great friend. I would enter the salon often worn down by the stresses of the week, tired and bedraggled. I would leave like Beyonce, flicking my hair and strutting like a diva ready to take on anything; I miss that.
I eventually pulled myself round, the constant support from my close network of friends and family, the totally amazing oncology nurses at the Sir Robert Ogden Macmillan centre and a friend’s blog actually pulled me back to reality. It’s only hair and in the big scheme of things I am very lucky.

Holding on to memories.
Amidst all of the above, during the summer an extraordinary human being and friend who had been a special part of my childhood and my adult life, died; he was having a bone marrow transplant following years of living with leukaemia. He was without doubt, exceptional. He was an amazing musician, played the Sax like it was part of his human form, a song writer and producer. He touched the lives of so many people in a positive way and he has left a large void that is hard to fill. In the last year of his life he did an amazing thing for a complete stranger, at a time when he was already unwell himself. He lived his life with love and passion and humour, signing off all his messages with ‘Love and sunshine’, that was John.

This photo taken by Mark Loraine, another of my very talented childhood friends (I’m surrounded by talent!) makes me smile so much. It was taken on Saltburn beach, one of my favourite places in the world and where I know John liked to surf. John left us all a legacy in his music that lives on. More than that he left us all with an insight of how to live our lives better. Since his passing there has been a swell of love, and a desire from those that were lucky enough to know him, to be more like John. He was kind, he lived his life with love, he gave to others generously, and he always, always made me smile.
Holding on to my career and holding on by my finger nails to life itself.
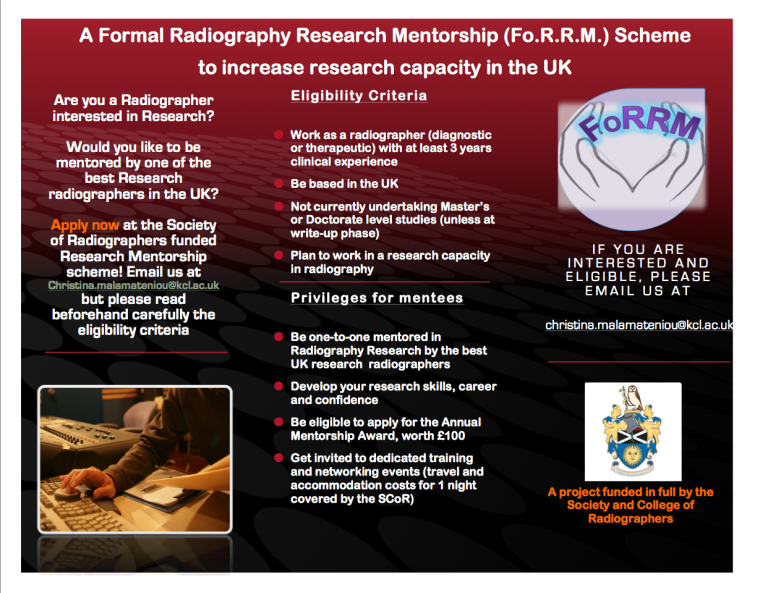
During the process of the standard cancer bad news, treatments, appointments, bloods, and procedures we have tried to maintain business as usual at home for our children. The usual life stresses still happen and we still have to deal with keeping on top of the school diary of organised events (Harvest festival, choir concerts, athletics competitions) as well as gymnastics training and competitions. Dealing with the accidental dropping of your daughter’s one and only school tie in the dog’s water bowl 2 minutes before you have to leave for school, or supporting our son through settling into a new job in a new city and finding a flat to live in that he can actually afford on a graduates pay, these all still need our attention. Add in that my husband is still working, still trying to make sure he gives his patients the care that they need, contributing to on-call to save adding burden to his already stretched colleagues. I am still trying to work when I am feeling well, because I believe my work is important, has worth and I am determined that my life will not be defined by my breast cancer diagnosis. I am a female academic, my career is already disadvantaged because I took a career break to have two children and I work part-time (and I wouldn’t have it any other way). But research funding applications don’t have sections where you can claim extenuating circumstances for having fewer peer-reviewed journal articles than your colleagues. I have cried lots (daily in the first month following diagnosis) worried about the future and whether I would be there for my children when they needed me, and whether I would be there for my husband; the thought of leaving him to cope alone in the future is horrendous, and too hard to bear some days.
We are still struggling to manage our lives through my cancer journey. We are trying to keep life as normal as possible for our daughter who is coping with her mum having cancer treatment brilliantly. But she has had a couple of wobbles in moments of quiet time where her thoughts have drifted to worries about my breast cancer and the future. She’s not the only one who worries about the future, David and I worry with every pain and twinge I experience that brings a fresh heart sink moment of “is this something I need to tell somebody about? is it bone pain?”


Throughout this difficult period for us I have been so proud of how our children have pulled together as a family, how they have supported us and each other; no words can express my love and pride for these guys.
What it all comes back to is love, kindness and support. I have been blessed with the most amazing support from friends, colleagues (actually I don’t see them as colleagues they are all my friends) and family. I can’t tell you how much this support has meant during this period. The messages that come at all times of day with no expectation of a reply, the gifts left for me without need for words of thanks, the hand drawn pictures, the art personalised for me, all because people care and they want to help. The friends who meet me for coffee, for food, for walks, who share of their time, who send me playlists to lift my spirits and keep me going, who cry with me when I’m down, who come up with ways to help me overcome the difficult weeks. To those people who perhaps have stepped out of their comfort zone to tell me they love my new hair cut (I’m not always sure they know it’s a wig or not, but it doesn’t matter) they can’t know the truly transformative impact it has on helping me cope.
I find myself saying thank you so often and it never seems enough, and I also doubt whether these amazing people realise quite how important all that they have and continue to do for me and how much their messages buffer the difficult stuff. It’s no exaggeration that they are the only reason I am able to move from holding on to moving on. I have pondered what I could give back to these selfless human beings who have done so much for me. The one thing I feel I can give to you is the insight that a cancer diagnosis bestows on you. Live your life with passion, with purpose, and with love. It is easy to let the drudgery of the negativity in the media, or in the narratives that some people express under the guise of fact, but which is in fact opinion, bring you down. I recall as a young qualified therapeutic radiographer an older staff member saying to me “I don’t understand why you young ones are in such a hurry to achieve everything, you have the whole of your lives, what’s the rush?” I never could quite align myself to that thinking, and here I am faced potentially with a shortened life expectancy. I am prone to quoting a bit of Shakespeare and not breaking this trend I thought I’d share this extract from The Tempest, spoken by Prospero, which I love, and more eloquently describes the fragility of life, and the reality that in an instance all that we hold close may simply disappear.
“And like the baseless fabric of this vision,
The cloud-capped towers, the gorgeous palaces,
The solemn temples, the great globe itself—
Yea, all which it inherit—shall dissolve,
And like this insubstantial pageant faded,
Leave not a rack behind. We are such stuff
As dreams are made on, and our little life
Is rounded with a sleep”.
The Tempest Act 4 scene 1.
The truth is we are all mortal, and none of us know when our time will be up or when our dreams will end, and so we must use the time we have with purpose, with love, with kindness and with passion. I’m trying to be more like my friend John every day, he truly lived his life.
So, while I’ve been holding on over the last few months, I’ve done so because of amazing people, and amazing love and I will continue to hold on to my beautiful family, my beautiful friends, and to beautiful memories. As I sign off this blog, I’d like to share with you this song written and produced by John (sung by James Arthur) and I invite you to join me (in a virtual sense) to dance around your home while I dance in the kitchen holding on to my amazing husband, as we have hung on to each other and will continue to hold on to each other through this whole journey, me attempting to replicate the grace of Oti Mabuse from Strictly, failing terribly but enjoying the dream.
Love and sunshine people (oh and still hoping for crisps).